16th October 2013
The MDT is taken for granted as the pre-eminent vehicle for delivering mental health care to patients. The close juxtaposition of multiple different explanatory models and modalities of intervention - each upheld in one or more of the various different professionals in the team - offers at least a structural aspiration towards integrated practice.
A typical MDT might consist of:
See How to speak to a... for advice on Mentalizing the positions and dilemmas that different professionals take, or face.
In reality teams are often faced with managing empty posts, or simply do not have the staffing levels to provide for more than occasional contact with other members of the MDT, so that a particular patient will primarily be managed by one or two workers, who may not have the benefit of multimodal training.
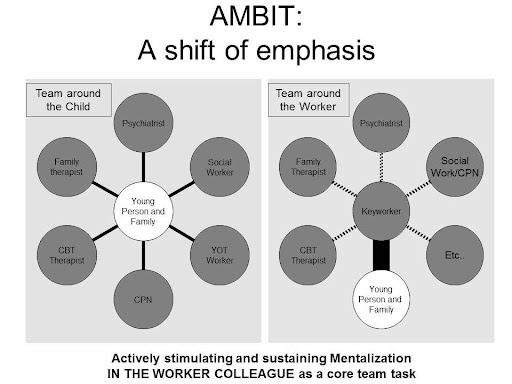
The AMBIT model of practice retains the MDT, but may place expertise at a 'Meta-level' - providing supervision rather than face-to-face management of the case. The shift is from a "team around the child" to a "team around the worker".
There is recognition that less Hard to reach groups will still respond well to the MDT approach to delivery, and this is demonstrably an effective way to deliver clinic-based services. In the IMP model of practice it is likely that an existing MDT (whose members would have completed the AMBIT training) would provide the supervisory input to a new AMBIT-influenced team
A typical MDT might consist of:
- SocialWorker
- Psychiatrist
- ClinicalNurseSpecialist (CPN)
- Psychotherapist
- OccupationalTherapist
- FamilyTherapist
- etc, etc...
See How to speak to a... for advice on Mentalizing the positions and dilemmas that different professionals take, or face.
In reality teams are often faced with managing empty posts, or simply do not have the staffing levels to provide for more than occasional contact with other members of the MDT, so that a particular patient will primarily be managed by one or two workers, who may not have the benefit of multimodal training.
The AMBIT model of practice retains the MDT, but may place expertise at a 'Meta-level' - providing supervision rather than face-to-face management of the case. The shift is from a "team around the child" to a "team around the worker".
There is recognition that less Hard to reach groups will still respond well to the MDT approach to delivery, and this is demonstrably an effective way to deliver clinic-based services. In the IMP model of practice it is likely that an existing MDT (whose members would have completed the AMBIT training) would provide the supervisory input to a new AMBIT-influenced team